
Our Thought Process
Using System Engineering, we perform these steps that allowed us to come up with the problem/solution statement. These steps also allows us to ensure that the solution we comes up with are innovative that addresses the stakeholder needs.
We chose to focus on the nursing domain because many James Dyson Award winners have tackled healthcare challenges reflecting the award’s emphasis on life-improving, practical design. Nurses are often first responders in critical situations, and their needs are central to ensuring effective patient care. Our solution aims to support them by addressing key gaps in workload management.
Step 1: Domain Analysis
When we have decided on the chosen domain (Healthcare - Nursing). We dived into the domain by understanding Nursing terminology and the current standard operating procedures (SOP). This helps us understand the domain better and enable us to craft questions to ask our relevant stakeholders.
What is Healthcare Sector?
What is Nursing?
The healthcare sector consists of businesses that provide medical services, manufacture medical equipment or drugs, provide medical insurance, or otherwise facilitate the provision of healthcare to patients.
What is their key roles & responsibilities?
-
Patient assessment
-
Care planning
-
Medication administration
-
Patient education
-
Monitoring and observation
-
Providing emotional support
-
Advocacy (patient’s right and needs)
-
Research & Development (R&D)
Healthcare profession focused on caring for individuals of all ages, families, groups, and communities, whether they are sick or well.
What is their core values?
-
Patient-Centered care
-
Evidence-based practice
-
Professional Judgement
-
Collaboration
What are the types of Nurses?
-
Registered Nurse (Normal)
-
Licensed (under supervision)
-
Advance (Specialised in an area)
Step 2: Stakeholder Interview
After we have an understanding of the domain. We proceed to the next step which is to find and interview relevant stakeholders from the domain to interview them. We asked non-leading questions, understanding their day to day work and any issues they may encounter. Evaluating all the issues that they encountering and selecting one that we are able to address.
Interviewed Stakeholder: Morgan, CGH Med Surgical Ward Student Nurse
What was your internship job's roles and responsibilities?
-
support nursing staff in delivering patient care
-
learn and apply clinical skills we learn in school
-
engage with patients
-
Morgan, cgh med surg ward, job title: student nurse
What is your day to day like?
-
help with monitoring vital signs and observing clinical procedures throughout the day
-
help patients with diaper change or repositioning for those with mobility issues
-
handover briefings at the start and end of shifts
-
assist patients with their adls
What are some frustrating things you experience?
-
lack of time to fully engage with patients due to the busy nature of the ward
-
nurses are usually too busy and overwhelmed with their own responsibilities to explain certain things
-
as students, we also lack the clinical skills to step in and help, so it can feel like we’re just getting in the way sometimes
-
patients might be hard to assist sometimes due to size
-
or lift for diaper change/clothes changing requiring more nurses.
-
ppe that cant stay in too long without getting really warm
Regarding the lifting or moving of heavy patients being a challenge, if we were to try and think of a solution for it, any sop we should take note of during these procedures?
-
there is sop but if you are planning to build smth, is more of the constraints of space and bedside considering that it is meant for use in the ward beside the patient
-
for us our sop is mostly hygiene related
What is the current way/sop to lift the patients up? and what is the minimum to maximum amount of nurses needed to lift a person up based on your experience?
-
we have a certain posture we have them move into if possible to assist us in moving them
-
currently if the nurse experienced, they one person can alr, the current intervention is for the nurse to wear a back brace to help prevent injury
If possible could you explain more on the posture, like what kind of posture is it?
-
something like this
-
but the leg below no need bend

We have identified these issues from the stakeholder interview and we have chosen to tackle the issue of lifting of large patients as it an issue that we are able to control.
Stakeholders Issues
- Lifting of large patients to change clothes and diaper
- Lack of clinical skills to help
- Customer Behaviors
- Unable to provide information to patients due to insufficient time
Step 3: Needs Formation and Validation
Upon getting the information from our stakeholders. We will re-visit the interview to form our needs statement, presenting it back to our stakeholder to validate if we capture it correctly.
Identified Needs
-
Need for a repositioning solution that is easy to utilize
-
Need for solution to be ergonomic and injury-preventive
-
Need for solution to be space-efficient for bedside use
-
Need for solution to be usable by 1 staff member
-
Need for tools or devices compatible with hygiene protocols
-
Need for an approach that minimizes manual labor without compromising patient dignity
-
Need for assistive devices or procedures that complement and align with existing SOPs
Validation Interview
As part of your day to day do you help to reposition or change diapers for the patients?
-
Most of the shift i will
-
Depends if i am in charge or not
When i interviewed some other nurses, they highlighted that they struggled to lift heavier and larger patients, needing more manpower to do so, do you agree with this statement?
-
Yes i agree
Right now at Sengkang General Hospital, what are the current practices you have in place when it comes to lifting heavier patients?
-
Usually for bed bound heavy pt , we always have 2 nurses to help out and using draws sheets to carry patients
Are there any SOP we have to keep in mind when designing a solution for this problem?
-
Make sure to have good posture when carrying pt to reduce back pains
What important features do you think the solution should have?
-
Bed at the right height and position for moving patients
For our solution, if it eliminates the strain on the nurses back, are there any other SOPs we should be aware of?
-
Patients pressure injury
Step 4: Literacy Review, Market Survey & Evidence
To ensure that the issue is accurate from what the stakeholder told us. We did more searching to find relevant articles or supporting documents that ensure us it was an actual need. We also search for existing solutions to understand their capabilities and limitations. With this in place, we can ideate an innovative solution
Workplace Injury


Based on these graph, over-exertion/strenuous is the 2nd top incident under Health & Social Services. The sector also have one of the highest musculoskeletal disorder cases.
Existing Solutions

SEABIRD Patient Turning Device Multifunctional U-Shaped Turning Pillow with Strap Waterproof Rest Nursing Tool Hemiplegia Paralyzed Bedridden Patient Turning Pillow Help The Elderly Turn Over

Patient Turning Device Belt For Bed Rails Elderly Adults Safety Hospital Beds For Home Use Transfer Belts For Lifting Seniors Multifunctional Turnover Bedridden Disability Prevention Bed Sore Aid Care

Ergotrics Solutions for Intensive Care Unit (ICU) and Operating Room
Current Limitations
-
Seabird and Patient Turning and existing solutions options seem to have a similar issue whereby there is a reliance on the patient to have some ability to pull themselves up slightly for these tools to be effective
-
The U-shaped turning pillow’s main issue is that it still relies on the patient to be able to somewhat position or bend their legs in order to fit into the U-shaped pillow. If they have painful joints or physical limitations, this can greatly hamper the effectiveness of this product.
-
Similarly, the Patient turning device belt also had an issue whereby the patient has to be able to hold themselves up for the strap to be properly fastened. If unable to do so, the belt wouldn’t be able to properly support the patient and be ineffective.
-
Ergotrics solutions are mainly targeted towards Intensive Care Unit (ICU) and the operating room. These means that they are not meant for general purpose uses. Each of their solution only targets a problem each, making it costly to target multiple solutions.
Step 5: Ideating a Solution
After we have gather our evidence to justify it is an actual need, and also did our market survey to understand the current capabilities and limitations with them. We are able to ideate a solution that addresses the limitations, while maintaining the current capabilities. We are also turning the stakeholder needs into requirement, allowing us to ideate potential solution to satisfy all needs.
Stakeholder Needs
- Need for a repositioning solution that is easy to utilize
- Need for solution to be ergonomic and injury-preventive
- Need for solution to be space-efficient for bedside use
- Need for solution to be usable by 1 staff member
- Need for tools or devices compatible with hygiene protocols
- Need for an approach that minimizes manual labor without compromising patient dignity
- Need for assistive devices or procedures that complement and align with existing SOPs
Current Market Limitations
- Expensive
- Multiple solutions addressing 1 problem individually
- Not widely adapted
- Requires third party's air pumper
- Not portable
- Requires a rail to be installed on the ceiling
Step 6: Diving Deeper
To allow us to ensure the solution is feasible, we also have to do more searching. This allow us to ensure that the items we need to procure for prototyping are available on the market.
Items we will need for Minimim Viable Product (MVP)
- Inflatable and Deflatable Air pump
- Inflatable Bolsters, Pillows and Head Rest
- Easy slip on sheets
- Tubing to connect all inflatables
- Valve to connect the tubings
As all the items needed are easily procurable for us, we deemed the solution is feasible. Allowing us to move forward to prototyping phase.
Step 7: Prototype/Proof of Concept
Once all the measures are taken into account. We sketched out the solution first for a low level prototype before using Solidworks to shape it out and move onto high level prototyping. We are able to start procuring required items to start on our prototyping phase.
Sketch

Solidworks Design


Actual Prototype (InflatAssist)

Before Inflation

After Inflation

Step 8: Stakeholder Validation
To evaluate the effectiveness of our prototype, we conducted a stakeholder validation session. Feedback was obtained through a brief interview and hands-on demonstration. Overall, stakeholders agreed that the solution fulfilled the intended objective of assisting patient rotation.
However, two key areas of concern were highlighted:
-
The time taken for the device to inflate.
-
The possibility of the patient shifting out of position during the process.
These insights are crucial as they highlight real-world limitations that could affect usability in a Hospital setting.
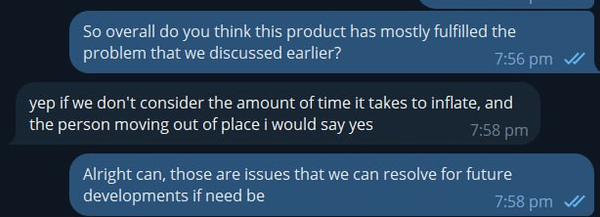
Stakeholder validation in progress. While the solution was generally well-received, feedback identified two main areas for improvement: inflation time and patient movement during use.
Step 9: Future Plans
As this marks the final iteration of our project, no immediate changes will be made to the prototype. However, the feedback received has informed several potential areas for future development:
-
Faster Inflation Mechanism: Exploring more powerful pumps or using Hospital beside air line if available, as an alternative to the current portable pump, which could significantly reduce inflation time.

-
Patient Positioning Solutions: Initially, we selected the EasySlide material, a microfiber (polyester) with padded layers and a specialized Ultra Low Friction (ULF) surface, to allow the device to be easily slid under the patient when needed. However, after testing and stakeholder interviews, we found that leaving the device permanently in place under each patient bed is more practical. As a result, in future iterations, we will consider replacing the EasySlide material with one that offers higher friction. This will help maintain patient positioning during inflation and reduce the risk of unintentional sliding.
-
Automated Valve Control:
-
At present, the valves are manually operated to inflate or deflate individual bolsters at specific intervals. In future iterations, these valves could be upgraded to an automated system that can be controlled via a device, allowing users to select patient positions and automatically inflate or deflate the corresponding bolsters.
-
Currently, the speed and pressure of airflow during inflation and deflation are manually regulated by adjusting the degree to which the valves are opened. This aspect can also be automated to precisely control and display the airflow rate and internal pressure of each bolster. This air pressure can also be controlled and regulated by the system for each
-

Conclusion
This project has taken us through a comprehensive and structured application of the systems approach, from domain analysis and stakeholder engagement to ideation, prototyping, and validation. By grounding our work in real-world needs and continuous feedback, we developed a solution that not only addresses a genuine issue in the nursing domain but also lays the groundwork for further improvement. While this marks the final iteration within the scope of our project, the insights gained and the positive stakeholder reception demonstrate the potential for real-world application and future development. We hope this serves as a meaningful contribution toward improving patient care through thoughtful and user-informed design.